Lab Daniel Giglio - HBOT Against Radiation Cystitis
Short description
Radiation against cancers in the pelvic area is effective, however, may lead to urinary bladder and bowel disturbances (radiation cystitis and proctitis, respectively) leading to poor quality of life. Hyperbaric oxygen therapy (HBOT) is effective in the treatment of radiation cystitis and proctitis, however, the treatment is time consuming for the patient and resource demanding. We are studying biomarkers that may identify which patients with radiation cystitis and proctitis that are helped by HBOT. Moreover, we are studying whether we can treat patients with a reduced number of HBOT treatments if we intervene at an earlier stage of radiation cystitis and proctitis
Hyperbaric Oxygen Therapy in the Prevention of Radiation Cystitis After Radiotherapy Against Tumours of the Pelvic Region
Background
Radiotherapy aimed at pelvic tumors, such as those in the uterine cervix, corpus, prostate, rectum, and urinary bladder, can cause severe side effects that significantly impact quality of life. These side effects include bowel and urinary urgency, frequency, hematuria, diarrhoea, vaginitis, and dyspareunia. Acute radiation cystitis occurs in about 50% of patients receiving curative intentionally radiation doses against tumours of the pelvic region. Chronic radiation cystitis after radiotherapy against tumours in the pelvic region is developed in around 10% of patients. At present, no biomarkers exist to predict which patients who are at risk to develop radiation cystitis. Chronic radiation proctitis occurs in 5-20% of patients undergoing pelvic radiotherapy. Radiation against gynaecological cancers may also lead to changes in the vaginal wall, reduced lubrication, difficulties conducting intercourse and dyspareunia. Few treatment options exist for patients developing chronic radiation cystitis, proctitis and vaginitis. Hyperbaric oxygen therapy (HBOT) has been shown to be effective against radiation cystitis and proctitis. Our research group has studied the effects of HBOT on the cellular level, in animal studies and in patients. We show in animal models of radiation cystitis that changes in the immune system and oxidative stress occur and that radiation-induced changes in the urinary bladder can be reversed by HBOT. Moreover, we show that the micturition reflex is sensitized in the radiated rat urinary bladder. Unpublished data from the group show in animal studies that HBOT may also reverse oxidative stress in the gynaecological tract. In a randomized phase 2-3 trial we demonstrated that HBOT may be effective in treating radiation cystitis, even in patients who had been suffering from the condition for several years. Results from the research group show that biomarkers within the immune system may predict which patients that will benefit from HBOT.
Methods
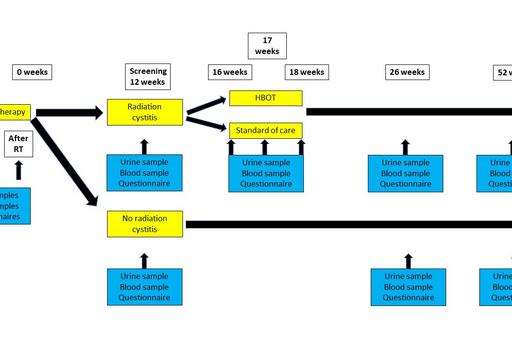
At baseline before radiotherapy, at the end of radiotherapy, at 12 weeks following radiotherapy, at 6 months and 12 months after start of HBOT/control treatment, patients will leave urine and blood samples for analysis with ELISA of an identified protein biomarker panel predicting clinical efficacy of HBOT. Moreover, we will test whether 20 sessions of HBOT against radiation cystitis/proctitis is enough if we intervene with HBOT already four months after radiotherapy instead of 40 sessions used today in clinical practice. Assessment of urinary, bowel and sexual function before and after HBOT will be assessed with questionnaires.

Significance
Radiation cystitis is a common side effect of radiotherapy against tumours in the pelvic region. HBOT has shown efficacy against the condition, however, at present studies suggest that 40 sessions are needed to treat this patient group leading to many visits to the health care for the patients and high costs. In the present study we will assess whether it is possible to prevent the development of radiation cystitis and reduce the number of treatments needed by intervening at an earlier stage of radiation cystitis. Moreover, we will validate whether a biomarker panel can identify the patient group with the best chance to have clinical efficacy of HBOT.
Collaborators at the University of Gothenburg
Daniel Giglio, Associate Professor, Principal Investigator, Department of Oncology, Institute of Clinical Sciences, Sahlgrenska Academy.
Helene Seeman-Lodding, MD, PhD, Associate Professor, co-Principal Investigator, Department of Anesthesia and Intensive Care Medicine, Institute of Clinical Sciences, Sahlgrenska Academy.
Lana Sallam, undergraduate student, Department of Oncology, Institute of Clinical Sciences, Sahlgrenska Academy.
Nicklas Oscarsson, MD, PhD, Department of Anesthesia and Intensive Care Medicine, Institute of Clinical Sciences, Sahlgrenska Academy.
Johan Mölne, MD, PhD, Associate Professor, Department of Laboratory Medicine, Institute of Biomedicine, Sahlgrenska Academy.